I have been living with type 1 diabetes for more than 30 years now and as long as I can remember, the HbA1c value was used as a gold star measuring stick in judging overall blood sugar control.¹ If an A1c was below 7%, most endocrinologists were satisfied.
However, with the increased use of continuous glucose monitors (CGM), additional data has allowed providers to now see a broader picture of how well-managed their patients’ blood glucose levels are. This is the value of Time In Range, or TIR for short.
Note: HbA1c is the best studied parameter that scientists were able to connect to long-term complication. However, research on TIR is ongoing and it becomes more and more obvious that increasing your TIR reduces the likelihood of diabetes complications [4]. However, there is more work to be done to prove the benefits of TIR over HbA1c in long term studies.
1. What does Time in Range mean?
Time in Range (TIR) indicates the percentage of how long your glucose value was within the target range during a defined period which can be multiple days up to months.² This number can sometimes be described as “hours in target range” as well. If a person has a TIR of 50%, that would indicate that your glucose levels were within the target range for an average of 12 hours on any given day.
Personal target ranges may vary from person to person, as best guided by your primary care provider, but official guidelines recommend that overall, glucose values should stay within 70 mg / dl and 180 mg / dl (3.9-10 mmol / l) for people with Type 1 and Type 2 diabetes.³
Brief sidebar for anyone who needs a diabetes 101 educational reminder:
The HbA1c shows the percentage of the “sugared” red blood pigment in the total hemoglobin content in your blood.⁶ Or, to put it simply, the sugar in your blood adheres to the red blood pigment (hemoglobin) a bit like cake frosting. This ‘frosting’ sticks as long as the red blood cells survive. Survival is an average of 8-12 weeks, but can vary from person to person.
2. Why is Time in Range so important?
In contrast to the HbA1c value, the Time in Range offers a few decisive advantages. Primarily, the A1c only represents the average glucose value over the past 2 to 3 months as a single snapshot. That means lower HbA1c does not necessarily mean that your glucose levels are better. But of course, you can achieve good HbA1c values despite having many hypos and hypers.
In fact, having a lot of dangerous hypos decreases your HbA1c. But a higher TIR automatically means a more stable glucose control with less time in hypos and/or hypers.
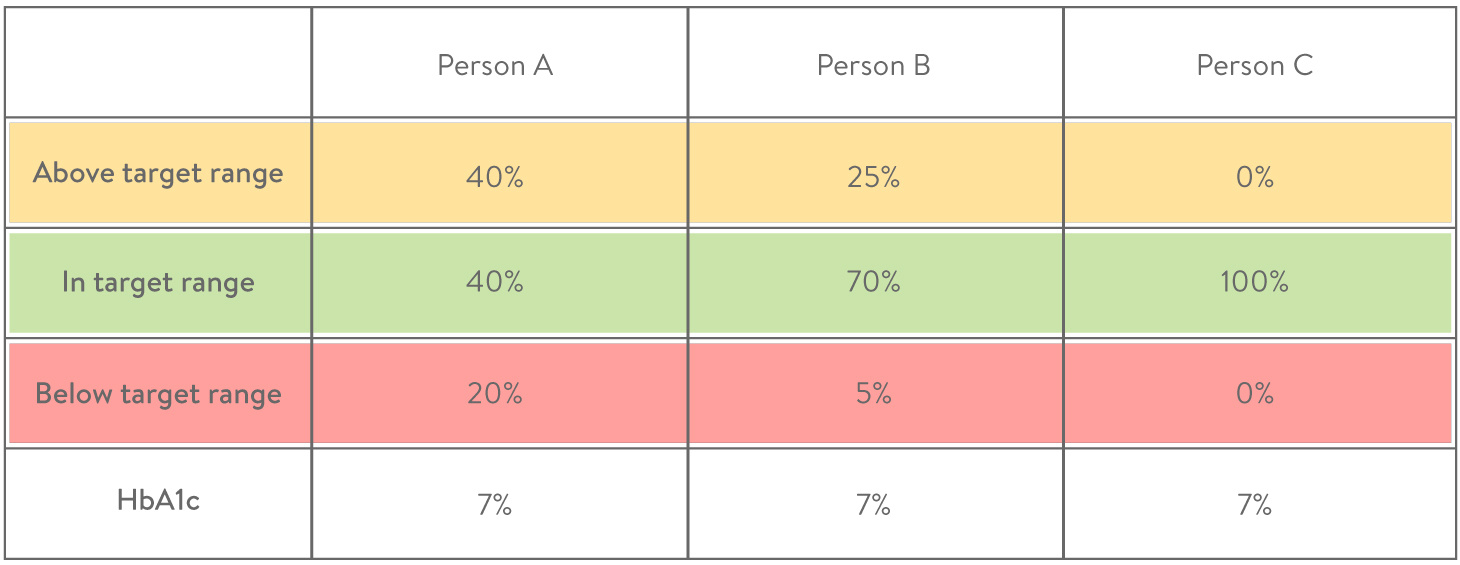
Want a fuller overview of your daily diabetes management? The following example shows that TIR tells you much better how good your glucose values are compared to HbA1c.
Here is an example:
Although all three people in the example above received a supposedly good Hb1Ac from their doctor, a closer look at the time spent in range shows a different picture. This information is vital in making those small, and sometimes constant, changes needed to live well with diabetes.
We now know that it’s not only permanently elevated BGs that risk long-term complications, but also fluctuating glucose levels. The more fluctuations over time, the more risk towards complications such as diabetic retinopathy or diabetic kidney disease.⁴
3. Relationship between TIR and risk of complications confirmed in studies
Scientists found that there is a strong connection between the time in range and the risk of diabetes complications.⁴ Some scientists even believe that TIR is the superior indicator of complications.⁵ The HbA1c is an indirect measurement of glucose in the blood, and is dependent on the renewal of the red blood cells which can vary from person to person. This makes the A1c a measure that can be influenced by various external factors.
As such, many are leaning towards the simplicity of TIR. The higher the time in the range percentage, the lower the risk of developing complications. The lower the TIR, the higher the glucose variability and thus the risk of possible complications.
Another great thing about the Time in Range value is that you can figure it out yourself! If you are a user of a continuous glucose monitoring at home, you do not have to go to a doctor or to a laboratory as you would with the HbA1c value. This, in conjunction with advances in telemedicine, makes the TIR an ideal part of your diabetic toolbox.
4. What is the optimal time in range target?
Most experts agree that the standard target range of 70-180 mg / dl (3.9-10 mmol / l) is best.⁷ However, personal considerations such as pregnancy, fear of hypoglycemia, or other health conditions may require individual adjustment of the target range on a temporary or ongoing basis. The target range should be determined individually together with your doctor.
Once you do set your range, try your best to be in that target range as much as possible while actively avoiding hypoglycemia. Progress comes slowly, so do not freak out when you leave your target range. Be cautious not to overreact and let your glucose level slowly get back to avoid strong hypos/hypers.
According to studies, the average time in range in people with diabetes is typically around 50% to 60%.² Based on the latest findings,⁷ Researchers at the ATTD Congress 2019 (Advanced Technologies & Treatments for Diabetes) made the following recommendations for people with type 1 and type 2 diabetes:
-
At least 70% of the day within 70 to 180 mg / dl (3.9-10 mmol / l)
-
Less than 4% of the day below 70 mg / dl (3.9 mmol / l)
-
Reduction of time over 180 mg / dl (10 mmol / l) per day
Most importantly, one should take care to set small but achievable goals.Focus on adjusting therapy settings, lifestyle etc step by step and use TIR as a feedback tool. And utilize any telemedicine options available to stay in close contact with your primary provider.
Just in case you ever wondered what the normal TIR is for a person without diabetes, a recent study figured that out. In the study, people without diabetes were monitored for 10 days with CGM systems.⁸
Result: 97% time in range with a target range of 70 to 140 mg / dl (3.9-7.8 mmol / l) and an average glucose value of 99 mg / dl (5.5 mmol / l) with only slight variation. Welcome to your new favorite factoid!⁹
5. How do I measure time in the target range?
In order to determine your personal time in range, you need your glucose data, which would be measured with a glucose sensor in the previous 14 days. If you are using a CGM system, the work is done for you since the CGM systems determine a glucose value around the clock giving you a consistent stream of measured values on average every 5 minutes.
Furthermore, most CGM (or other Flash Glucose Monitoring) systems automatically determine the time in the range and make this information readily available to you either on the reader, on an app, or in the respective evaluation software.
With a standard blood glucose meter, using individual fingersticks, the endeavor is unfortunately more complex. In order to obtain a similarly consistent database, you would have to determine each data point by pricking your finger every 5 minutes.
For those brave caffeine-addicted warriors who feel dedicated enough to try this level of insanity, the TIR can be manually calculated as follows:
(Values in target area / total amount of values) x 100 = amount of values in target area in %.
Pro Tip:
In the mySugr app, you can define your individual target area in the settings and have it displayed in the blood sugar graph on the home screen. The target area you defined is a little darker. So you can see at a glance how the day is developing in terms of time in range.
How do I use the Time in Range to optimize therapy?
While you should always discuss therapy adjustments with your diabetes care provider in advance before making any changes, Time in Range has proved to be an ideal monitor for your diabetes therapy. Use it to check if changes to your therapy have the desired effect. Possible scenarios:
-
You notice that your carbohydrate factor is somehow off. You can contact your diabetes team and make a quick adjustment. After 14 days, you look at your time in range and find that this little tweak has increased your TIR by 3%!
-
You struggle with high BG values after a meal and you suspect the pre-meal bolus as the culprit. Reach out to your care provider and discuss adjusting that preprandial time. In a week or so, view the TIR percentage to determine whether you are on the right path!
-
The Time in Range gives you information about whether your efforts are going in the right direction in a short amount of time. No more waiting for the next appointment with the doctor to look forward to your HbA1c value.
Again, small adjustments. You should do this in a structured manner and coordinate all steps with your diabetes team. This is the only way the Time in Range value can develop its superpower.
-----------------------------------------------------------------------------------------------------------------------
Sources:
- D. M. Nathan, et al. 2014.The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care, [online]. Available at: https://pubmed.ncbi.nlm.nih.gov/24356592/
- DiaTribe, 2019. Time-In-Range. [webpage] Available at: https://diatribe.org/time-range [Accessed 24/03/21].
- American Diabetes Association. 2021. 6. Glycemic Targets: Standards of Medical Care in Diabetes. Diabetes Care, [online]. Available at: https://care.diabetesjournals.org/content/44/Supplement_1/S73
- Vigersky R. A., McMahon C., 2019. The Relationship of Hemoglobin A1C to Time-in-Range in Patients with Diabetes. Diabetes Technology and Therapeutics, [online]. Available at: https://pubmed.ncbi.nlm.nih.gov/30575414/.
- M. A. L. Gabbay, et al. 2020. Time in range: a new parameter to evaluate blood glucose control in patients with diabetes. Diabetology and Metabolic Syndrome, [online]. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7076978/
- e Medicine Health, 2020. Hemoglobin A1c Test (HbA1c). [webpage] Available at: https://www.emedicinehealth.com/hemoglobin_a1c_hba1c/article_em.htm [Accessed 24/03/21].
- T. Battelino, et al. 2019. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care, [online]. Available at: https://care.diabetesjournals.org/content/42/8/1593
- Mass Device, 2020. Abbott touts real-world data around FreeStyle Libre system. [webpage] Available at: https://www.massdevice.com/abbott-touts-real-world-data-around-freestyle-libre-system/ [Accessed 15/04/2021].
- Lily Nichols RDN., 2020. CGM Experiment: What I Learned as a Non-Diabeteic from Wearing a Continuous Glucose Monitor. [webpage] Available at: https://lilynicholsrdn.com/cgm-experiment-non-diabetic-continuous-glucose-monitor/ [Accessed 15/04/2021].
The mySugr website does not provide medical or legal advice. mySugr blog articles are not scientific articles, but intended for informational purposes only.
Medical or nutritional information on the mySugr website is not intended to replace professional medical advice, diagnosis or treatment. Always consult a physician or health care provider with any questions you may have regarding a medical condition.