You're strolling home after a long day, you feel wiped out and pretty hungry. A quick meal and bumming around on the couch sounds perfect. At least that was the plan... But suddenly your brain screams 'hypo' and the next thing you know you wake up to strange people looking down at you. It's your worst nightmare; a low blood sugar that requires emergency assistance.
If I'm too slow or get caught off guard
Hypos make us feel lousy, shaky, and just bad.
We often just want to feel better again! And most of the time, we can handle it ourselves with a bit of juice, glucose, or whatever we choose. But sometimes we might need a little help from friends, family, or co-workers. Even then, it's usually not too bad.
But what if we're out alone and get caught off guard, or if the low happens too fast, and we lose our senses or pass out?
What exactly happens while we're "not there" to experience it?
I was really curious, so I started asking some questions.
Quick and effective help – usually
I interviewed some first responders, paramedics, and firefighters here in Austria and asked them about their experiences helping us Monster Tamers. I'm sure there are many differences according to regional practices, licensing, and guidelines, but I think it's still useful to share what I learned.
What happens, should you pass out, is actually pretty uneventful, save the worry and concern of those around you.
Hopefully someone sees that you need help and calls quickly. There is another article's worth of discussion on this point alone, but for today, let's assume rescue has been called and are on their way. In most populated areas, it shouldn't take more than a few minutes for them to arrive.
Medical ID
Upon arrival, they will check if you are breathing and then blood pressure. They are also scanning for any sort of medical ID – a bracelet, a necklace, maybe even a tattoo. Those I interviewed mentioned this without my prompting, which I found reassuring, and also said they check thoroughly as soon as possible.
That being said, I've also heard from others who say rescuers missed very visible and plain medical IDs. If you're not responsive the next check is blood sugar. And BAAAAM – low blood sugar confirmed.
Treating
If you are completely unconscious then a glucagon rescue injection or glucose solution IV is necessary, and not everyone can administer these treatments. A glucose solution IV, for example, can only be given by an emergency doctor or a paramedic who is qualified to start an IV (it requires venous access).
Paramedics or first responders without these skills can administer glucose gels, but only if you are conscious. This makes sense, right? If you are unconscious and people start putting stuff in your mouth, you could choke on it.
A glucose solution IV usually works very quickly. Often in a matter of minutes, you'll wake up and your monster will have calmed down.
Once you're awake and starting to feel better, another blood sugar check is done. If your BG is back to normal you can decide if you want to go to the hospital or not. The emergency doctor involved will also be very involved in this decision.
If your BG does not come back up to normal after a few minutes you'll be transported to the nearest hospital. You'll be checked from top to bottom and given more glucose until you're back up to normal.
Every clue helps
A tip for those calling rescue on our behalf: Take a quick survey of our stuff – even a quick look in our purse or pockets – and let the emergency center know if you see any medical looking stuff. A blood glucose meter, a bottle of glucose tabs, maybe even an emergency card. It's all really helpful information to the emergency center.
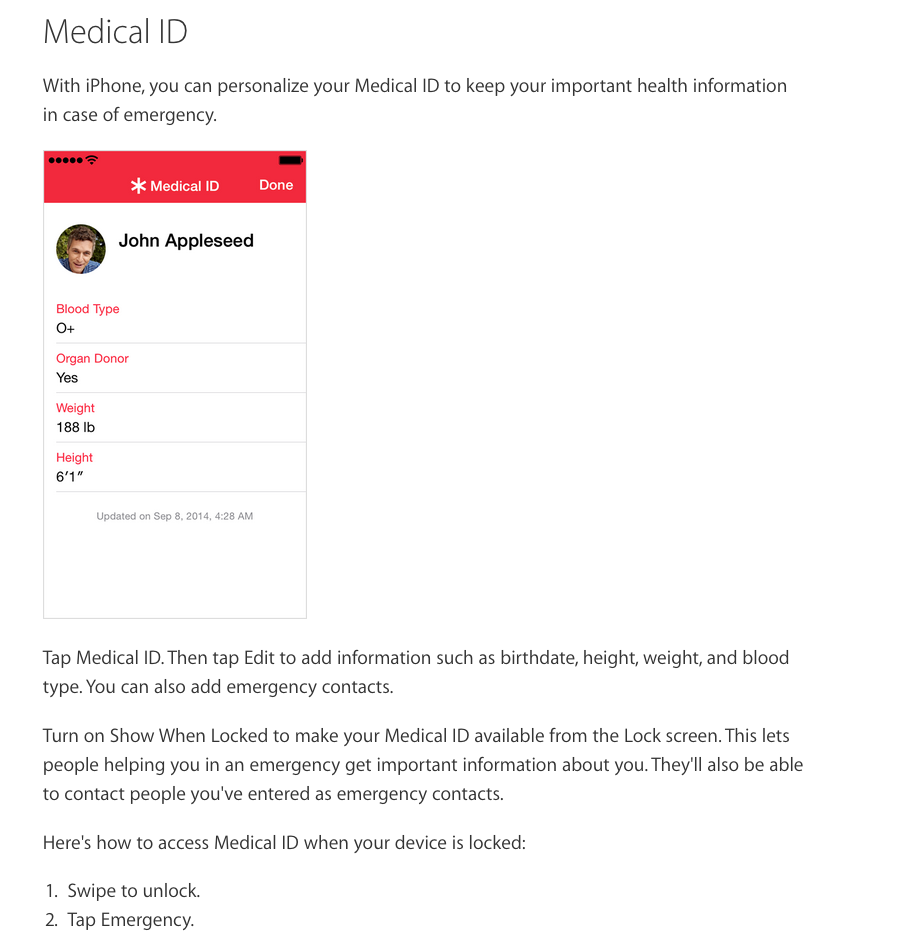
Turn on our phones, too. Is there an ICE contact (ICE stands for In Case of Emergency) or Emergency information on the home screen? Did you know iPhone users with iOS 8 or higher can add emergency info to their lock screen?
Any bit of information can help, so it doesn't hurt to check while you're calling. But please don't delay – time is critical!
Nothing to be embarrassed about
A bad hypo is nothing to be ashamed of. None of us are immune to the risk of low blood sugars. It can happen to any of us and it's important to remember that. The important thing is that you are okay.
You should definitely document what happened and talk about it with your doctor as soon as possible. We need to make sure that diabetes monster doesn't throw any more unauthorized parties!
The mySugr website does not provide medical or legal advice. mySugr blog articles are not scientific articles, but intended for informational purposes only.
Medical or nutritional information on the mySugr website is not intended to replace professional medical advice, diagnosis or treatment. Always consult a physician or health care provider with any questions you may have regarding a medical condition.





