Injecting insulin is part of the daily routine for most people with diabetes and has become an automated process.
However, this might lead to “favorite injection spots” that are overused. In this article we’ll cover insulin injection tips and explain the role of the needle length!

1. Where Is The Insulin Injected?
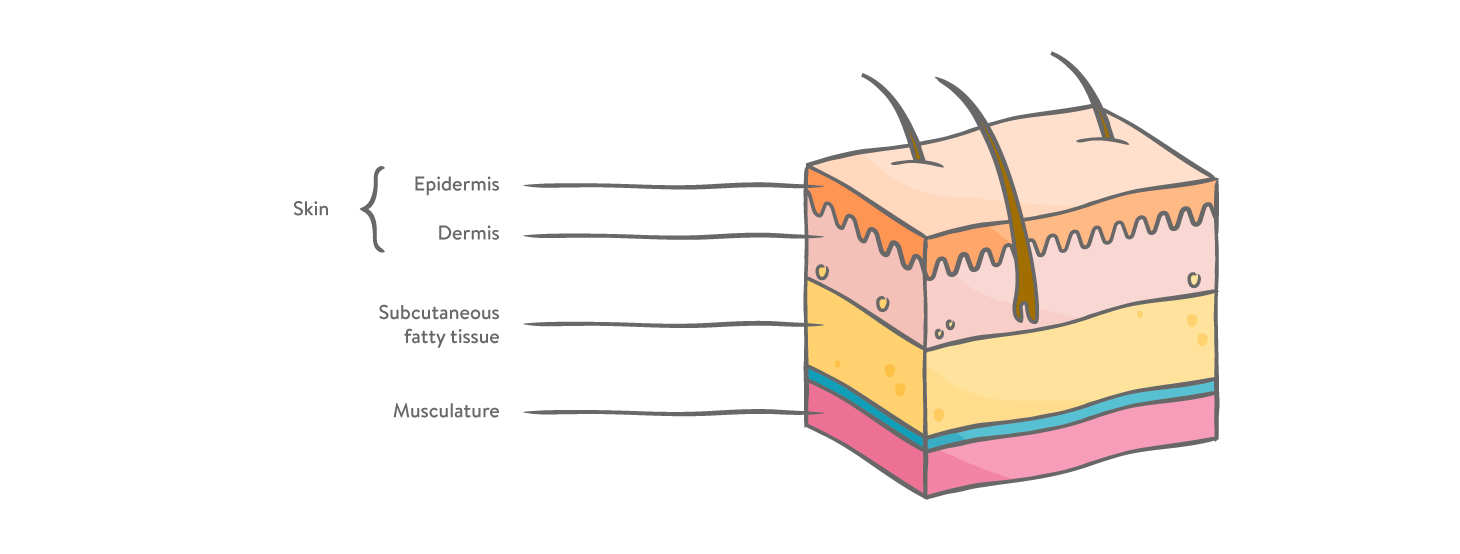
For best effectiveness, insulin has to be absorbed into the subcutaneous fatty tissue. Afterwards, it is distributed throughout the body to do its work. In adults, this fatty tissue layer is only 2.0 - 2.5 mm beneath the skin's surface. In children and adolescents it can be slightly less.¹ Not so thick, huh?
To inject the insulin into this optimal location, the needle must pass through the top layer of skin, but not too deep. The aim of the injection is to get the insulin under the skin, and if possible, avoid backflow, pain or bleeding.
The structure of the skin:
2. How Long Should the Needle Be?
Did you know, waaaay back in the day, insulin needles could run as long as 12mm? That’s nearly a ½ an inch long!
Lucky for us, needles are much shorter and thinner than they used to be. Even needles that are 10mm long for adults and 8mm long for children are now considered too long.² They increase the risk of insulin being transported to the muscles where it doesn’t belong.
Injections into muscle are painful and the insulin absorption is less controlled than it is in the subcutaneous fat tissue. This can result in hypoglycemia.³ Furthermore, medical studies have shown that needle length makes no difference to HbA1c values or the amount of hypos or hypers!⁴ Yay Science!
So now, using a tiny 4 mm needle, you can achieve your HbA1c targets, avoiding potentially painful and risky muscle injections while managing your diabetes.⁵
Shorter and thinner needles are now considered safer and more tolerable - also for the psyche. That’s why - also for adults: short 4mm pen needles are the safest needles to prevent injections into the muscle.²
Injections should be done vertically (without folding your skin) and are therefore long enough to get through the skin layer into the subcutaneous fat tissue.⁶
After triggering the injection by pressing the button on your pen, it’s important that you leave the needle in your skin for about 10 seconds to allow the insulin to be distributed optimally.⁶
3. Where Are The Best Injection Sites?
As we mentioned above, you want to inject your insulin into a good pocket of subcutaneous fat. Abdomen, thighs, and buttocks are often ideal injection areas for people with diabetes.⁶ These locations typically provide the best options for optimal insulin absorption.
For manual shots, it’s recommended that you create a fold of skin to inject the insulin to avoid injecting into muscle tissue.⁶ Pen users don’t always need to do this, especially if the needles are the super short 4mm length. Either way, below are a few tips to help the process of injecting run smoothly.
- Most fast-acting insulins can be injected into the subcutaneous fatty tissue;
- Long-acting insulins can be injected into either the abdomen or the thigh.
- When using the abdominal area for injections, inject at least 2 cm away from your belly button.
- If using cloudy basal insulin, remember to swirl it around at least 20 times before injecting it, and aim for the outer thigh or buttock area.
- After insulin has been injected using either a pen or a needle, keep the needle in your skin for about 10 seconds. This helps avoid the insulin leaking back out.
4. Why Do I Have to Vent Pen Needles?
Remember to “vent” or “prime” your needles prior to use! This means you point the needle away from you and inject 2-3 units into the air to remove any air bubbles in the dose (we like to call that an air shot).⁶ You know you have successfully primed when a few drops of insulin come out of the needle.
Venting has two advantages:
First of all, you can ensure that you will inject the exact amount of insulin and prevent injecting air by accident. Furthermore, it might happen from time to time that - against the official recommendations - needles are used 2-3 times. This can cause insulin to crystallize in the needle and block it - something you would notice when venting the needle.
5. Which Injection Sites Should I Avoid?
Since the target is to inject insulin where it can be most evenly absorbed into the bloodstream, the following are all big no-no’s and should be strictly avoided:⁷
- moles
- stretch marks
- cuts, scrapes, or scars
- bruises
- veins
6. Why Is Changing Injection Spots So Important?
The main rule with injection sites is simple: Do not inject continuously into the same spot. Repeat injections in the same spot on the body can contribute to the development of lipohypertrophy. Lipohypertrophy is a medical term that refers to a lump under the surface of the skin caused by an accumulation of subcutaneous fat and/or scar tissue which can become thick or hard.⁶
Lipohypertrophy lumps are not only a cosmetic problem. They can lead to absorption issues with your insulin due to an increase in connective tissue. This can lead to an unclarified hyper- but also hypoglycemia. A higher insulin dose is often required as a result. Furthermore, lipohypertrophy lumps can be prone to irritation and infection as well.
7. How Often Should Injection Areas Be Checked?
It is, of course, better to avoid lipohypertrophy in the first place. But sometimes these things just happen. Therefore, regular injection site checks are a wise move.⁷ Your diabetes team should check your injection sites at least twice a year.
This is typically done at your regular check-up and doesn’t require an additional doctor visit. You can also do it yourself! Using a mirror, you can look for asymmetrical elevations at your favorite injection points. You can also run your fingers along the area and feel for lumps and bumps under the skin’s surface.
Most of these problems will resolve themselves but it’s still a good idea to make a note of your injection sites so you can be on the lookout for signs of infection.
8. What is Injection Rotation?
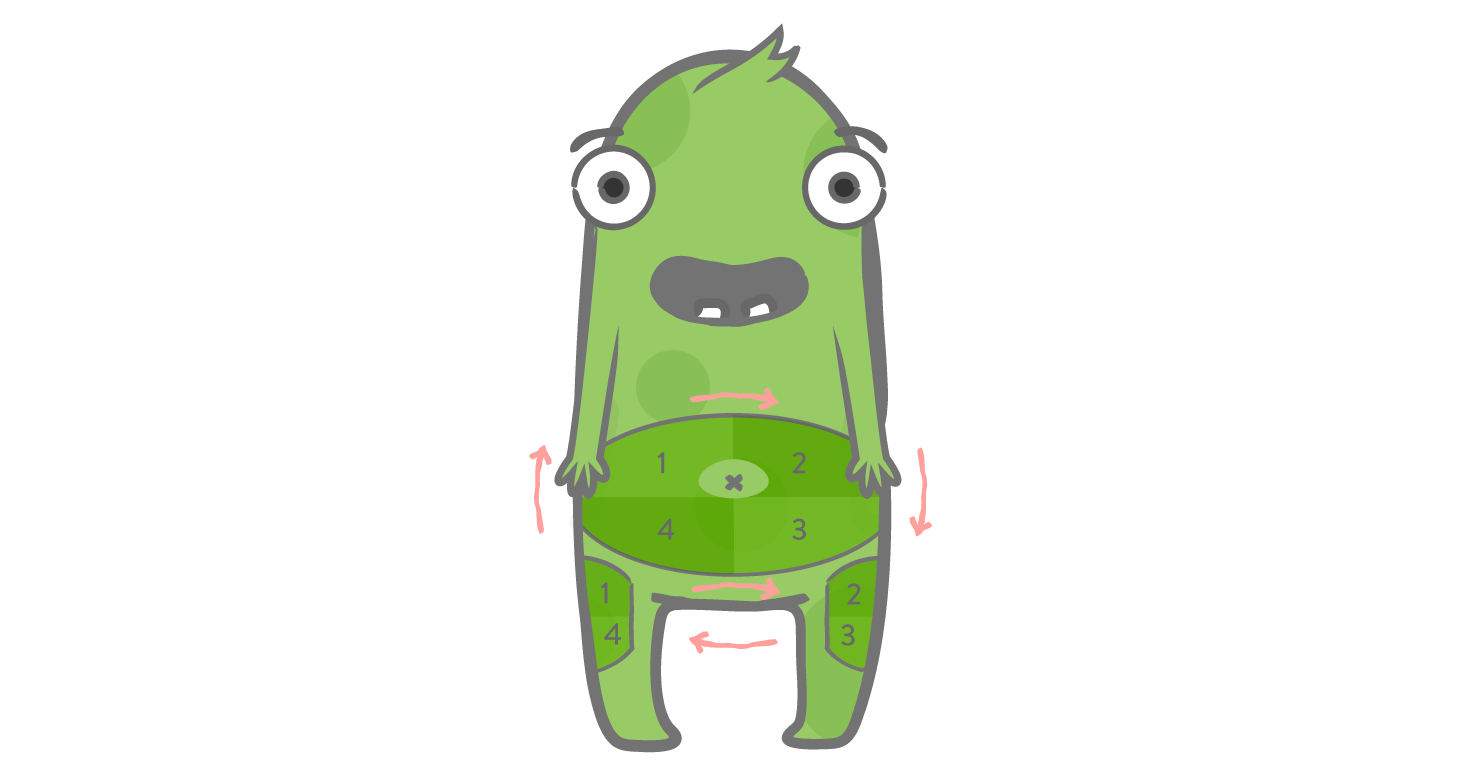
One simple way to avoid injecting insulin into the same spot over and over is to rotate your injection sites. The process is fairly simple. You divide your injection locations (stomach, buttocks, thighs, etc.) into 4 quadrants.
Rotating clockwise within them, use a different location each time you inject. Using a rotation approach lowers the risk of lipohypertrophy and encourages smoother/faster healing in between injections.⁷
By the way, don’t worry if you are bleeding a little bit after injecting. This can often be caused by hitting a little blood vessel which has no impact on the effect of your injected insulin.
If you worry about forgetting, there are easy charts and even temporary tattoos you can get to help you keep track! Tipp: you can also track/tag your infusion set change in the mySugr app, in case you are using an insulin pump.
9. What About Insulin Pump Users?
Similar to the injection needles, the trend for insulin pump catheters has also moved towards shorter cannulas to infuse insulin into the subcutaneous fatty tissue. These should also be rotated and moved frequently.⁷
Some insulin pumps utilize tiny steel needles, while others use a flexible teflon cannula. Your pump manufacturer and care team can guide you specifically, but the typical rule is that pump sites should be changed every 2-3 days at the latest.

Sources:
- Gibney, M.A., Arce, C.H., Byron, K.J., Hirsch, L.J., 2010. Skin and subcutaneous adipose layer thickness in adults with diabetes at sites used for insulin injections: implications for needle length recommendations. Current medical research and opinion. [online] Available at: https://pubmed.ncbi.nlm.nih.gov/20429833/.
- Very Well Health, 2020. How Needle Size Affects Diabetes Control. [webpage] Available at: https://www.verywellhealth.com/diabetes-and-pen-needles-1087295 [Accessed 21/01/21].
- Medical News Today, 2020. What are the side effects of insulin therapy? [webpage] Available at: https://www.medicalnewstoday.com/articles/323387 [Accessed 21/01/21].
- Bergenstal, R.M., Strock, E.S., Peremislov, D., Gibney, M.A., Parvu, V., Hirsch, L.J., 2015. Safety and efficacy of insulin therapy delivered via a 4mm pen needle in obese patients with diabetes. Mayo Clinic Proc. [online] Available at: https://pubmed.ncbi.nlm.nih.gov/25662503/.
- Fitter 4 Diabetes, 2020. Helping to achieve HbA1c targets. [webpage] Available at: https://www.fitter4diabetes.com/pages/helping-to-achieve-hba1c-targets [Accessed 21/01/21].
- Diabetes.co.uk, 2019. How To Inject Insulin. [webpage] Available at: https://www.diabetes.co.uk/insulin/how-to-inject-insulin.html [Accessed 21/01/21].
- Diabetes Forecast, 2016. Do’s and Don’ts of Injection Site Rotation. [webpage] Available at: http://www.diabetesforecast.org/2016/sep-oct/injection-site-rotation.html [Accessed 21/01/21].
The mySugr website does not provide medical or legal advice. mySugr blog articles are not scientific articles, but intended for informational purposes only.
Medical or nutritional information on the mySugr website is not intended to replace professional medical advice, diagnosis or treatment. Always consult a physician or health care provider with any questions you may have regarding a medical condition.





